Connect With Us

Prevention of Heel Spurs

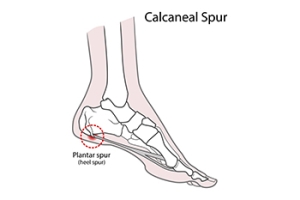
Heel spurs are bony growths that develop on the underside of the heels. They are visible on X-rays, and can protrude up to half an inch. While heel spurs themselves are generally not painful, they often accompany conditions such as plantar fasciitis and Achilles tendonitis, which also lead to heel discomfort. These spurs can be caused by overstretching the tissue connecting the heel and the ball of the foot or by the gradual wear and tear of the protective membrane covering the heel bone. To prevent heel spurs, it is important to wear well fitting shoes, maintain a healthy weight, and have a gait, or walking style check. Treatment options may include stretching exercises or taping to alleviate stress on muscles and tendons. Wearing shoe inserts or orthotic devices for additional support and comfort may also help. If you have a heel spur, and especially if it is associated with pain, it is suggested that you make an appointment with a podiatrist for a proper diagnosis and treatment.
Heel spurs can be incredibly painful and sometimes may make you unable to participate in physical activities. To get medical care for your heel spurs, contact Jeffrey Rosenblatt, DPM from New York. Our doctor will do everything possible to treat your condition.
Heels Spurs
Heel spurs are formed by calcium deposits on the back of the foot where the heel is. This can also be caused by small fragments of bone breaking off one section of the foot, attaching onto the back of the foot. Heel spurs can also be bone growth on the back of the foot and may grow in the direction of the arch of the foot.
Older individuals usually suffer from heel spurs and pain sometimes intensifies with age. One of the main condition's spurs are related to is plantar fasciitis.
Pain
The pain associated with spurs is often because of weight placed on the feet. When someone is walking, their entire weight is concentrated on the feet. Bone spurs then have the tendency to affect other bones and tissues around the foot. As the pain continues, the feet will become tender and sensitive over time.
Treatments
There are many ways to treat heel spurs. If one is suffering from heel spurs in conjunction with pain, there are several methods for healing. Medication, surgery, and herbal care are some options.
If you have any questions feel free to contact our office located in Brooklyn, NY . We offer the latest in diagnostic and treatment technology to meet your needs.
Heel Spurs
Heel spurs are the result of calcium deposits that cause bony protrusions on the underside of the heel. Heel spurs are usually painless, but they have the potential to cause heel pain. Heel spurs tend to be associated with plantar fasciitis, which is a condition that causes inflammation of the band of connective tissue that runs along the bottom of the foot. They most often occur to athletes whose sports involve a lot of running and jumping.
Some risk factors for developing heel spurs include running and jogging on hard surfaces, being obese, wearing poorly fitting shoes, or having walking gait abnormalities.
It is possible to have a heel spur without showing signs of any symptoms. However, if inflammation develops at the point of the spur’s formation, you may have pain while walking or running. In terms of diagnosis, sometimes all a doctor needs to know is that the patient is experiencing a sharp pain localized to the heel to diagnose a heel spur. Other times, an x-ray may be needed to confirm the presence of a heel spur.
Heel spurs can be prevented by wearing well-fitting shoes that have shock-absorbent soles. You should also be sure that you are choosing the right shoe for the activity you want to partake in; for example, do not wear walking shoes when you want to go on a run. Additionally, maintaining a healthy weight can be beneficial toward preventing heel spurs, as it will prevent an excess amount of pressure being placed on the ligaments.
There are a variety of treatment options for people with heel spurs. Some of these include stretching exercises, physical therapy, shoe inserts, or taping and strapping to rest stressed muscles and tendons. If you have heel pain that lasts longer than a month, don’t hesitate to seek help from a podiatrist. Your doctor can help you determine which treatment option is best for you.
Definition, Causes, and Treatment of Clubfoot

Clubfoot, a congenital condition, impacts the development of a newborn's foot or feet, leading to an abnormal position. The foot is turned inward and downward, resembling the shape of a golf club, hence the name. While the exact cause is not always clear, both genetic and environmental factors can play a role. During pregnancy, abnormal positioning of the baby's feet in the womb can contribute to developing clubfoot. Early treatment of this condition is important and generally begins within weeks of birth. The Ponseti method, a non-surgical approach involving gentle manipulation and casting, is a common treatment. Braces are used to maintain correction after the casting phase. In some cases, surgery may be necessary. Timely intervention and comprehensive treatment enable children with clubfoot to lead active, fulfilling lives. If your child has been born with clubfoot, it is strongly suggested that you contact a podiatrist who can determine what the best course of treatment is to pursue.
Some foot conditions may require additional professional care. If you have any concerns, contact Jeffrey Rosenblatt, DPM of New York. Our doctor can provide the care you need to keep you pain-free and on your feet.
Rare Foot Conditions
The majority of foot conditions are common and can be treated by a podiatrist. Standard diagnostic procedures are generally used to identify specific conditions and treatment can be rendered. A podiatrist also treats rare foot conditions which can be difficult to diagnose and may need extra attention and care.
There are many rare foot conditions that can affect children. Some of these can include:
- Freiberg’s disease
- Kohler’s disease
- Maffucci syndrome
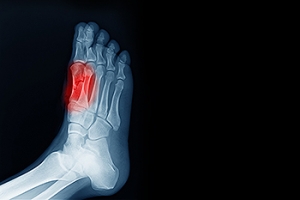
Freiberg’s disease - This can be seen as a deterioration and flattening of a metatarsal bone that exists in the ball of the foot. It typically affects pre-teen and teenage girls, but can affect anyone at any age. Symptoms that can accompany this can be swelling, stiffness, and the patient may limp.
Kohler’s disease - This often targets the bone in the arch of the foot and affects younger boys. It can lead to an interruption of the blood supply which ultimately can lead to bone deterioration. The patient may limp or experience tenderness, swelling, and redness.
Maffucci syndrome - This affects the long bones in a child’s foot leading to the development of abnormal bone lesions. They are benign growths and typically develop in early childhood and the bones may be susceptible to breaking.
A podiatrist can properly diagnose and treat all types of rare foot conditions. If your child is affected by any of these symptoms or conditions, please don’t hesitate to call our office so the correct treatment method can begin.
If you have any questions please feel free to contact our office located in Brooklyn, NY . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.
Rare Foot Conditions
A podiatrist will be able to address a variety of rare foot conditions, particularly the ones that affect children. The most common are Kohler’s disease, Maffucci syndrome, and Freiberg’s disease. They can be properly diagnosed by having an X-ray taken, but in more serious cases an MRI may be needed. Kohler’s disease generally affects younger boys and bone deterioration may result from an interruption of blood supply. Children who have Kohler’s disease may find relief when the affected foot is rested, and a special boot is worn. Benign growths in the long bones of a child’s foot may lead to the development of bone lesions, and this is known as Maffucci syndrome. People who have this condition find mild relief when custom-made orthotics are worn. Freiberg’s disease targets the ball of the foot and can typically affect pre-teen and teenage girls. The metatarsal bone becomes deteriorated and flattened, and common symptoms include swelling and stiffness. A cast is often necessary to wear with this disease as it can help to reduce existing pain. Erythromelalgia is a rare foot condition, and its cause is unknown. Symptoms of this disease can include intense burning pain and the feet may appear red or feel warm. Relief may be found when the affected foot is immersed in ice water. It can also be beneficial to elevate the foot frequently. If your child complains of foot pain, it is strongly suggested that you consult with a podiatrist who can diagnose and treat rare foot conditions.
Tips for Preventing Falls Among the Elderly

Falling presents a significant threat to the well-being of older adults, often leading to severe injuries, hospitalization, and sometimes death. With age, the risk of falling can increase as a result of health issues such as arthritis, muscle weakness, and poor balance. Tips for preventing falls can start with evaluating prescription medications that may affect balance. It is beneficial to create a safer home environment by keeping pathways clear of cords and removing loose carpets or rugs. Installing additional lighting in dim areas and staircases, and placing nightlights in key locations are effective fall prevention techniques. Additional methods can consist of decluttering living spaces, especially around stairs and narrow passageways, and installing handrails on both sides of steps, indoors and outdoors. Put grab bars near the toilet and bathtub, and use non-slip mats in the bathroom. Choose shoes with secure soles and proper back support, avoiding loose slippers or socks. A podiatrist can aid in the prevention of falls through assessments of balance, strength, and walking gait. For more information, it is suggested that you make an appointment with this type of doctor who can guide you toward living in a safe environment.
Preventing falls among the elderly is very important. If you are older and have fallen or fear that you are prone to falling, consult with Jeffrey Rosenblatt, DPM from New York. Our doctor will assess your condition and provide you with quality advice and care.
Every 11 seconds, an elderly American is being treated in an emergency room for a fall related injury. Falls are the leading cause of head and hip injuries for those 65 and older. Due to decreases in strength, balance, senses, and lack of awareness, elderly persons are very susceptible to falling. Thankfully, there are a number of things older persons can do to prevent falls.
How to Prevent Falls
Some effective methods that older persons can do to prevent falls include:
- Enrolling in strength and balance exercise program to increase balance and strength
- Periodically having your sight and hearing checked
- Discuss any medications you have with a doctor to see if it increases the risk of falling
- Clearing the house of falling hazards and installing devices like grab bars and railings
- Utilizing a walker or cane
- Wearing shoes that provide good support and cushioning
- Talking to family members about falling and increasing awareness
Falling can be a traumatic and embarrassing experience for elderly persons; this can make them less willing to leave the house, and less willing to talk to someone about their fears of falling. Doing such things, however, will increase the likelihood of tripping or losing one’s balance. Knowing the causes of falling and how to prevent them is the best way to mitigate the risk of serious injury.
If you have any questions, please feel free to contact our office located in Brooklyn, NY . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Falls Prevention
Elderly Americans are very susceptible to falls as they get older. Everyone experiences decreases in flexibility, balance, strength, and the senses as they age. This correlates to some eye-opening statistics. 1 in 4 Americans aged 65 and older fall each year. An elderly American is being treated for a fall in an emergency room every 11 seconds. In light of these striking statistics, one can see the importance of taking steps to prevent falls.
Finding an exercise program for the elderly is an excellent way to reduce the likelihood of falls. Look for an exercise program that improves strength and balance. Elderly people who live a more sedentary lifestyle, with little physical activity, are at an increased risk of falling. Wearing well-fitted footwear that provides good foot support and cushion will help prevent falls from poorly fitted shoes. Talking to a podiatrist about your susceptibility to falls and about inspecting your prescriptions will help to avoid any medication that could make falls more likely. Due to a decline in the senses among the elderly, having your eyes and hearing checked is recommended.
Around half of all falls occur in the household. Removing tripping hazards in the home and making it more accommodating to older persons can significantly reduce falls. Some notable household changes include increasing lighting around the house, installing grab bars in the shower and bathroom, and making sure the floor is clear of clutter. Other smart options include installing a shower chair, using rubber-bottomed rugs, and placing railings on both sides of stairwells.
Finally, discuss with a doctor and your family about your fear of falling. This will help to increase awareness among the population on the need for fall prevention. A lack of awareness on the matter, and a downplaying of importance are what increase the risks of falling. Following these tips can help to reduce the risk for yourself and your loved ones.
Lyme Disease and the Feet

Lyme disease, often transmitted by ticks, can bring about various symptoms that affect the feet and other parts of the body. While fever, fatigue, and rashes may signal its presence, a definitive diagnosis requires careful consideration of symptoms and circumstances. If one has been in wooded or grassy areas during tick season, it is possible to contract Lyme disease. Lyme disease's early signs, such as fever, chills, headache, fatigue, and muscle pain, can mimic a severe cold. Knee swelling is common, and joint pain may migrate across the body. As the disease progresses, headaches, Bell's palsy, and joint pain can intensify, and rare complications like heart involvement or mental health issues may arise. Shooting pains, numbness, or tingling in the hands and feet may be felt. It is suggested that you manage pain and inflammation and focus on your overall well-being to aid in healing. If you suspect you have Lyme disease, it is suggested that you make an appointment with a podiatrist for an accurate diagnosis and effective management.
When dealing with systemic disease of the feet, it is extremely important to check the affected areas routinely so that any additional problems are caught quickly. If you have any concerns about your feet and ankles contact Jeffrey Rosenblatt, DPM from New York. Our doctor will assist you with all of your podiatric needs.
Systemic Diseases of the Feet
Systemic diseases affect the whole body, and symptoms usually are displayed in the feet. This condition can make a patient’s ability to walk unbearable. Systemic diseases include gout, diabetes mellitus, neurological disorders, and arthritis.
Gout – is caused by an excess of uric acid in the body. Common symptoms include pain, inflammation, and redness at the metatarsal/phalangeal joint of the base big toe. Gout can be treated by NSAIDs to relieve pain and inflammation, and other drugs that lower the acid levels in the body.
Diabetes mellitus – is an increase in the level of blood sugar that the body cannot counteract with its own insulin. Failure to produce enough insulin is a factor in Diabetes.
Diabetes of the Feet
Diabetic Neuropathy – may lead to damaged nerves and affect the feet through numbness and loss of sensation.
Peripheral Vascular Disease – can restrict the blood flow to the feet, and often times lead to amputation of the feet.
If you have any questions please feel free to contact our office located in Brooklyn, NY . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Systemic Diseases of the Foot
There are several systemic diseases, or diseases that affect the whole body, that either display symptoms in the feet or affect the health of the feet. Common systemic diseases that affect the overall health of the feet, and the patient’s ability to walk comfortably, include gout, diabetes mellitus, neurological disorders, and arthritis, among others.
In gout, which is caused by an excessive buildup of uric acid in the body, the most common symptoms of pain, inflammation, and redness occur at the metatarsal/phalangeal joint at the base of the big toe. Any excess levels of uric acid crystallize and are deposited in tendons, joints, and surrounding bone and muscle tissue. Gout is commonly treated with NSAIDs to relieve pain and inflammation and other drugs to lower uric acid levels in the body. Gout most commonly affects those who are overweight, have low protein diets and lead a more sedentary lifestyle.
Diabetes mellitus is an increase in the level of blood sugar in which the body cannot counteract with naturally occurring insulin in the body. The three types of diabetes, Type I, Type II and Gestational Diabetes, are all signs the body is either not producing enough insulin or is not efficiently using the insulin that is produced. Gestational diabetes only affects women who are pregnant and have never, prior to pregnancy, exhibited symptoms of the disease.
There are two main issues that affect the feet that are commonly caused by diabetes. They include diabetic neuropathy and peripheral vascular disease. Diabetic neuropathy can lead to damaged nerves and affect the feet through numbness and loss of sensation. Peripheral vascular disease restricts the flow of blood to the foot and can, in extreme cases, lead to the necessity of amputating the foot. Peripheral issues that are caused by diabetes and can affect the foot include athlete’s foot, nail infections, corns, blisters, bunions, severe dry skin, plantar warts and ingrown toenails. These can all be attributed to the decrease of blood flow to the foot.
Neurological disorders and rheumatoid arthritis can also have severe impact on the health of the feet. Neurological disorders can affect the nerves in the main structure of the foot and cause loss of sensation and possible decreased muscle response. Rheumatoid arthritis can affect the bones and joint structures of the foot, making it impossible to walk normally without serious pain.
All systemic diseases that affect the foot can effectively be treated to minimize joint and muscle damage if they are diagnosed early and treated with medication and lifestyle therapy. Diabetes patients must monitor their blood sugar levels and work with their physician to keep their levels as close to normal as possible. Rheumatoid arthritis patients should work with their physician to ensure the proper medications are being taken to reduce the amount of damage to the joints of the body.
How to Find Relief From Sesamoiditis

Sesamoiditis is a painful condition that affects the sesamoid bones, which are two small bones in the foot located beneath the big toe joint. These bones play a crucial role in providing leverage for the tendons and muscles, allowing smooth movements during activities such as walking and running. Sesamoiditis occurs when these bones become inflamed, which generally happens from overuse, repetitive impact, or excessive pressure. The primary symptom of sesamoiditis is sharp pain beneath the big toe, which worsens during weight-bearing activities. Treatment for sesamoiditis involves rest and taking anti-inflammatory medications to reduce pain and inflammation. Wearing supportive footwear, padding, and orthotic inserts can alleviate pressure on the affected area. In severe cases, a podiatrist may recommend immobilization with a walking boot or cast to allow the sesamoid bones to heal properly. Proper management and early intervention are essential to prevent long-term complications and ensure a swift recovery from sesamoiditis. If you are afflicted with sesamoiditis, it is strongly suggested that you contact a podiatrist who can help you to manage this condition.
Sesamoiditis is an unpleasant foot condition characterized by pain in the balls of the feet. If you think you’re struggling with sesamoiditis, contact Jeffrey Rosenblatt, DPM of New York. Our doctor will treat your condition thoroughly and effectively.
Sesamoiditis
Sesamoiditis is a condition of the foot that affects the ball of the foot. It is more common in younger people than it is in older people. It can also occur with people who have begun a new exercise program, since their bodies are adjusting to the new physical regimen. Pain may also be caused by the inflammation of tendons surrounding the bones. It is important to seek treatment in its early stages because if you ignore the pain, this condition can lead to more serious problems such as severe irritation and bone fractures.
Causes of Sesamoiditis
- Sudden increase in activity
- Increase in physically strenuous movement without a proper warm up or build up
- Foot structure: those who have smaller, bonier feet or those with a high arch may be more susceptible
Treatment for sesamoiditis is non-invasive and simple. Doctors may recommend a strict rest period where the patient forgoes most physical activity. This will help give the patient time to heal their feet through limited activity. For serious cases, it is best to speak with your doctor to determine a treatment option that will help your specific needs.
If you have any questions please feel free to contact our office located in Brooklyn, NY . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.